Neural Implants: Technology, Applications, and Future Prospects
Updated On: November 13, 2025 by Aaron Connolly
What Are Neural Implants?
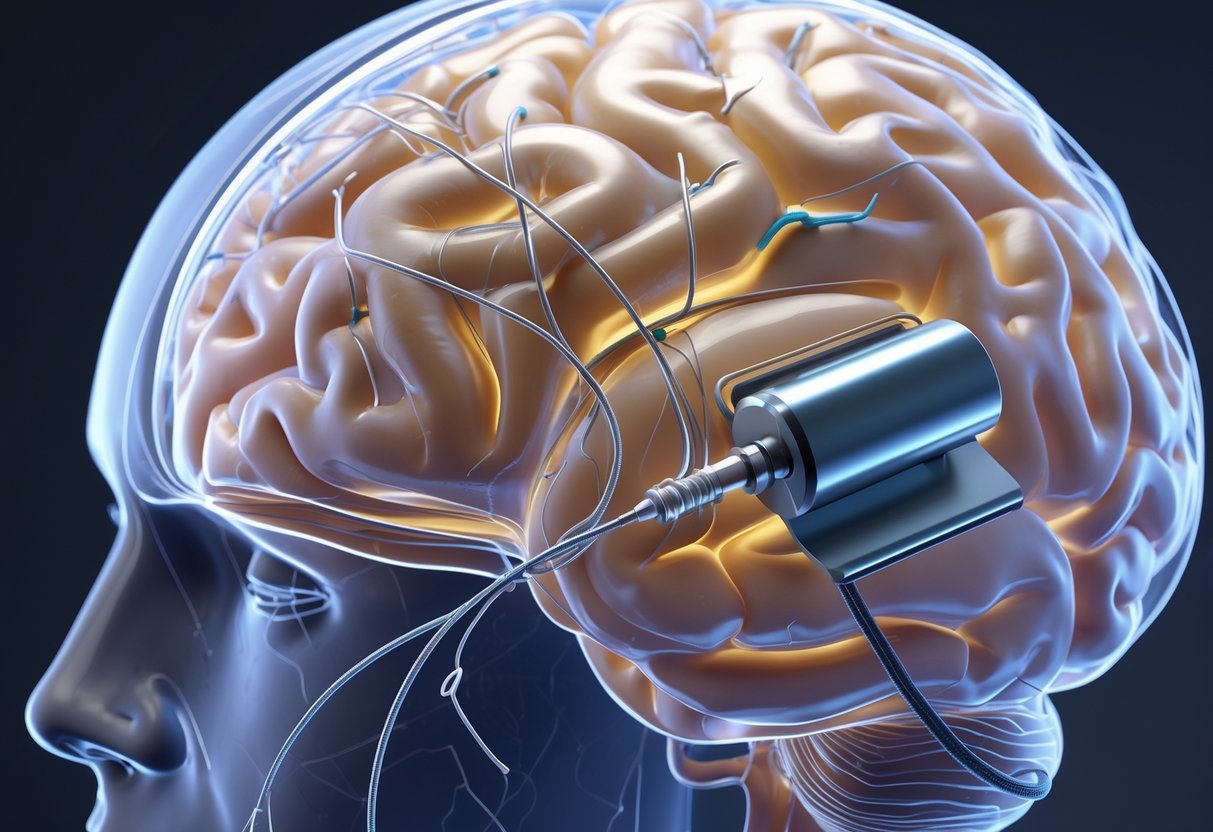
Neural implants are electronic devices that surgeons place into the brain, spinal cord, or nervous system to record neural signals, stimulate neurons, or restore lost functions.
These devices pick up the electrical impulses that neurons use to communicate. They can either monitor this activity or send their own electrical signals to change how the nervous system behaves.
Key Components and Mechanisms
Neural implants have several key parts working together. Electrodes are the core—they’re tiny conductive materials that touch neural tissue directly.
The electrodes link up with a signal processor that interprets the electrical activity from neurons. This processor decodes patterns of neural signals into usable information.
Most implants need a power source, usually a battery or a wireless charging setup. The battery has to be small enough to fit inside the body but still powerful enough to keep the device running.
A transmitter moves information between the implant and external devices. This feature lets the implant talk to computers, prosthetic limbs, or other medical equipment.
Modern implants rely on biocompatible materials to lower the body’s immune response. These materials help keep scar tissue from forming around the implant, which could mess with its function over time.
Types of Neural Implants
Deep brain stimulation (DBS) implants are probably the most established kind. They treat conditions like Parkinson’s disease, epilepsy, and essential tremor by sending electrical pulses to certain brain areas.
Spinal cord implants give people with paralysis a shot at regaining movement. They stimulate the spinal cord below the injury, and some patients can stand or walk a bit thanks to this tech.
Cochlear implants restore hearing by skipping over damaged parts of the ear and stimulating auditory nerves directly. Over 700,000 people use them worldwide.
Brain-computer interface (BCI) implants let people control external devices just by thinking. Researchers have helped paralyzed patients move computer cursors and robotic arms using these systems.
Vagus nerve stimulators treat depression, epilepsy, and other conditions by stimulating a major nerve that connects the brain to vital organs.
How Neural Implants Interface with the Nervous System
Neural implants tap into the electrical language of the nervous system. Neurons send messages through electrical impulses that fire in patterns—sort of like Morse code.
Recording neural activity means putting electrodes near neurons to detect these signals. The implant picks up tiny voltage changes when neurons fire.
Stimulation works the other way—the implant sends small electrical pulses to neurons, making them fire in chosen patterns. This can override faulty circuits or bring back lost connections.
The brain’s plasticity really helps here. The nervous system adapts and learns to work better with the device, so performance usually improves over time.
Signal processing algorithms decode complicated neural activity into commands that external devices can actually use. Modern implants can even tell the difference between different movements or intentions.
This interface builds a direct path between thoughts and technology. It bypasses damaged parts of the nervous system to restore function or even add new abilities.
How Do Neural Implants Work?
Neural implants interact with the brain’s electrical signals using tiny electrodes that can both record and stimulate nerve activity.
These devices turn brain signals into digital commands for external tech, and they also send electrical pulses back to influence neural circuits.
Signal Detection and Interpretation
Neural implants pick up the brain’s electrical activity through specialized electrodes placed close to neurons.
When nerve cells fire, they create small electrical impulses, and the implant’s sensors capture them.
These raw neural signals look like a mess of electrical patterns. It’s a bit like listening to thousands of conversations at once—the implant needs to sort through the noise for something useful.
The device uses advanced algorithms to decode these patterns. Every thought or movement intention has its own unique electrical signature.
If you imagine moving your right hand, the brain activity looks different than if you imagine speaking. The implant learns to recognize these differences over time.
Modern systems can pick up signals from single neurons or groups of cells. This level of detail allows for more precise interpretation of what the user wants.
Stimulation and Recording Techniques
Neural implants mainly do two things: they record natural brain activity, and they deliver electrical stimulation to specific brain regions.
Recording techniques use microelectrodes that are thinner than a human hair. These electrodes sit very close to neurons but don’t damage the surrounding tissue.
Deep brain stimulation sends carefully controlled electrical pulses to targeted brain areas. This can override abnormal activity or restore proper communication between regions.
The stimulation needs careful calibration. Too little current does nothing, but too much can cause side effects or even tissue damage.
Some implants do both jobs. They record neural activity to figure out what’s happening, then provide stimulation to fix problems or boost function.
Integration with External Devices
The implant connects to external computers that process neural signals in real time. This setup creates a direct communication pathway between the brain and assistive technologies.
A small transmitter, usually under the skin, sends wireless signals to external processors. That means no wires have to pass through the skull.
The external system translates brain signals into digital commands. Users can control computer cursors, robotic arms, or communication devices just by thinking.
Machine learning helps these systems get better as you use them. The more someone uses the implant, the better it gets at understanding their specific patterns.
Some systems even send feedback back to the brain. They can stimulate nerves to create artificial sensations, so users can “feel” what their prosthetic limbs are touching.
Brain-Computer Interfaces (BCIs) and Neural Implants
Brain-computer interfaces turn electrical signals from the brain into commands that control external devices.
These systems now let paralyzed patients move robotic arms, type messages, and even speak through computer-generated voices.
Definition of BCIs
A brain-computer interface picks up electrical signals from brain cells and converts them into digital commands. These signals happen when neurons fire as we think about moving or speaking.
Invasive BCIs use electrodes placed right on or in brain tissue. They record signals from individual neurons or small groups of cells.
Non-invasive BCIs read brain activity through the skull using methods like EEG. These signals are weaker and less precise than invasive ones.
Most invasive systems use Utah electrode arrays. These little silicon chips have up to 100 needle-like electrodes that poke into brain tissue by a few millimeters.
Electrocorticography (ECoG) puts flat electrode grids on the surface of the brain. This causes less tissue damage, but it doesn’t pick up as many detailed signals as the deeper electrodes.
Modern BCIs process neural signals in real time using AI algorithms. Machine learning helps them decode tricky brain activity and turn it into specific actions.
Role in Assistive Technologies
BCIs mainly help people with severe paralysis from spinal cord injuries, stroke, or conditions like ALS. These patients have normal brain function but can’t control their muscles.
Motor BCIs read signals from the motor cortex when patients imagine moving their arms or hands. The system translates these thoughts into cursor movements or robotic arm commands.
Researchers have shown that patients can control computer cursors with about 90% accuracy after training. Some people now type at speeds of 40 words per minute just by thinking.
Speech BCIs decode intended speech from brain signals. Patients with locked-in syndrome can generate computer speech by thinking about what they want to say.
In recent trials, a paralyzed woman controlled a digital avatar that spoke with her own pre-recorded voice. The system decoded her intended speech at 78 words per minute.
Prosthetic devices controlled by BCIs let patients grab objects and do daily tasks. One person even drank coffee with a robotic arm controlled by their thoughts.
Recent Advances in Brain-Computer Interfacing
Clinical trials now test BCIs in people’s homes instead of just labs. Some participants use these systems on their own for months, and they don’t need daily recalibration.
Wireless BCIs got rid of the cables connecting the brain to computers. Patients can move around freely and still control prosthetic devices or communication systems.
Companies like Synchron created endovascular BCIs that are inserted through blood vessels. This avoids open brain surgery but still records useful neural signals.
Multi-electrode arrays with thousands of recording sites now provide more detailed brain signals. These high-res systems improve accuracy and cut down training time.
AI advances let BCIs adapt to each patient’s unique brain patterns. Modern systems learn and get better over weeks of use.
Some studies have shown stable BCI performance for over three years in human patients. That kind of reliability makes these devices much more practical for daily life.
Speech BCIs can now decode complex sentences and even emotional tone from brain signals. Maybe future systems will restore natural conversation for people who can’t speak.
Applications for Restoring Motor and Sensory Functions
Neural implants bring life-changing solutions for people who have lost critical abilities. These devices can restore movement after paralysis, let people control prosthetic limbs, bring back hearing with cochlear tech, and even return vision through retinal stimulation.
Restoring Movement After Paralysis
Neural implants can get around damaged spinal cord pathways and restore movement in paralyzed patients. They record signals straight from the motor cortex when someone thinks about moving.
The implants pick up neural activity and turn it into commands for computers or external devices. People with complete paralysis can control computer cursors, wheelchairs, or robotic arms just by thinking.
Current capabilities include:
- Controlling computer interfaces for communication
- Operating wheelchairs and mobility devices
- Directing robotic assistance systems
- Activating muscle stimulation devices
Researchers are working on combining brain implants with electrical muscle stimulation. This combo could help people with partial paralysis regain some natural movement by reactivating their own muscles.
The technology works best for people with spinal cord injuries who still have a healthy motor cortex. Brain damage from stroke is trickier and needs different solutions.
Prosthetic Control and Sensory Feedback
Modern neural interfaces let users control prosthetic devices directly through brain signals. People can operate artificial limbs with surprising precision by just thinking about certain movements.
Advanced prosthetics now provide sensory feedback to the nervous system. Users can actually feel what their artificial limbs touch, which makes a huge difference in daily life.
Key prosthetic advances:
- Multi-finger hand movements
- Pressure and texture sensation
- Temperature detection
- Natural grip adjustments
Combining motor control and sensory feedback makes the experience feel more natural. Some users even say the prosthetic feels like part of their body, not just a tool.
Training usually takes a few months before users get smooth control. Most people start with simple open-and-close functions, then move on to more complex tasks.
Cochlear Implants and Hearing Restoration
Cochlear implants are probably the most successful neural prosthetic so far. They bypass damaged inner ear structures and directly stimulate the auditory nerve.
The implant turns sound into electrical signals that the brain interprets as hearing. Over 700,000 people worldwide use cochlear implants to get back functional hearing.
How cochlear implants work:
- External microphone captures sound
- Processor converts sound to digital signals
- Transmitter sends signals to internal implant
- Electrodes stimulate auditory nerve fibers
Most users get good speech understanding within six months of activation. Kids who receive implants early can develop almost normal language skills.
Cochlear implants work best for people with severe hearing loss who still have working auditory nerves. Results really depend on the cause of hearing loss and how long someone was deaf before getting the implant.
Retinal and Visual Prostheses
Retinal implants give hope for restoring sight in some types of blindness. These devices stimulate remaining retinal cells or the optic nerve to create visual perceptions.
Current systems offer basic light perception and shape recognition, not detailed vision. Users can spot movement, identify large objects, and move around familiar places more safely.
Visual prosthetic types:
- Epiretinal implants: Placed on the retinal surface
- Subretinal implants: Positioned under damaged photoreceptors
- Cortical implants: Target visual processing areas directly
The Argus II retinal prosthesis was one of the first approved devices. Users usually see patterns of light spots that represent visual info from a camera system.
Training is a must for learning how to use these artificial visual signals. Most people need months of practice before they can use the information effectively in daily life.
Treating Neurological Disorders with Neural Implants

Neural implants are changing the way we treat brain conditions that impact millions. These devices send electrical signals to specific brain regions, helping people manage symptoms of epilepsy, Parkinson’s disease, depression, and even early-stage dementia.
Epilepsy and Seizure Control
Doctors and researchers have made big strides in using neural implants to detect and stop seizures before they get out of hand. Modern devices rely on artificial intelligence to spot early warning signs in brain activity.
How seizure control works:
- Implants keep an eye on electrical patterns in the brain.
- AI algorithms pick up on abnormal activity in just seconds.
- The device sends targeted stimulation to block full seizures.
- Treatment only kicks in when necessary, not all the time.
Right now, epilepsy implants can cut seizure frequency by 50-70% for folks who don’t respond to meds. The responsive neurostimulation system sits under the scalp and hooks up to electrodes near seizure hotspots.
Key benefits include:
- Fewer emergency hospital runs
- Better quality of life for patients and families
- Lower risk of sudden death from seizures
Closed-loop systems are in the works too. These learn each patient’s unique seizure patterns, and early clinical trials look even more promising.
Management of Parkinson’s Disease
Deep brain stimulation has become a go-to treatment for Parkinson’s when meds aren’t doing the trick anymore. Surgeons place electrodes in specific brain areas that control movement.
The procedure targets spots like the subthalamic nucleus or globus pallidus. Electrical pulses help bring brain activity back to normal and cut down the abnormal signals behind Parkinson’s symptoms.
Improvements patients typically see:
- Less tremor and muscle stiffness
- Better balance and walking
- Reduced need for medication
- Improved sleep
Modern implants for Parkinson’s use rechargeable batteries that last 15-25 years. Doctors can tweak stimulation settings wirelessly with external controllers.
Treatment works best for:
- Motor symptoms like tremors and rigidity
- People who respond to levodopa
- Patients without major cognitive decline
Researchers are developing adaptive stimulation, which changes throughout the day. These smart implants adjust based on how active the patient is and when they take meds.
Addressing Depression and Mood Disorders
Doctors are testing neural implants for tough cases of depression that don’t respond to therapy or meds. The idea is to target brain circuits that control mood.
Deep brain stimulation for depression focuses on areas like the subcallosal cingulate cortex. Early results look promising for people with severe, long-standing depression.
Current research findings:
- 40-60% of patients show significant improvement
- Benefits usually build up over several months
- Treatment often works alongside therapy and meds
- Side effects are mostly manageable
Another option is the vagus nerve stimulator. This device sits under the skin of the chest and sends regular pulses to brain regions involved in mood.
Treatment considerations:
- Reserved for severe cases that haven’t improved with other treatments
- Requires careful patient selection and close monitoring
- Long-term studies are still underway
- Insurance coverage isn’t consistent everywhere
Closed-loop systems that detect mood changes through brain signals are in early stages. These could one day provide more personalised stimulation based on each person’s emotional patterns.
Applications in Alzheimer’s Disease and ALS
Early research suggests neural implants might help with memory and movement in neurodegenerative diseases. Scientists are studying how brain stimulation affects memory loss and muscle control.
For Alzheimer’s, implants target memory-related networks. Deep brain stimulation of the fornix region may slow cognitive decline in mild cases.
Alzheimer’s research areas:
- Improving sleep to reduce brain toxin buildup
- Boosting memory consolidation during rest
- Slowing down early-stage disease
- Supporting remaining cognitive skills
ALS research is looking at brain-computer interfaces that bypass damaged motor neurons. These systems read movement intentions straight from the brain.
ALS applications include:
- Moving computer cursors and typing on keyboards
- Controlling communication devices with thoughts
- Directing robotic arms and wheelchairs
- Helping people stay independent as the disease progresses
Some teams are working on implants that stimulate healthy motor pathways to keep muscles working longer. When combined with stem cell therapy, these approaches might slow ALS progression.
Current limitations:
- Most treatments are still experimental
- We need more long-term data
- High costs make access tough
- Surgery comes with real risks
Deep Brain Stimulation (DBS) Techniques
DBS delivers precise electrical pulses to specific brain regions through implanted electrodes. Doctors use this technique to treat movement disorders like Parkinson’s disease, and it’s showing real potential for depression and other neurological issues.
Mechanism of Action
DBS uses thin platinum-iridium electrodes to send electrical impulses right to targeted brain areas. The system has three main parts: electrode leads in the brain, extension wires, and a pulse generator under the chest skin.
The electrical current doesn’t destroy brain tissue. Instead, it changes how brain cells talk to each other. This helps control the abnormal activity behind symptoms.
Modern electrode designs offer better control than before:
- Cylindrical electrodes: Four contacts spaced along the wire
- Directional electrodes: Segmented contacts that steer current in certain directions
- Adjustable settings: Doctors can fine-tune voltage, frequency, and pulse width
The pulse generator acts like a brain pacemaker. It sends electrical signals at frequencies between 130 and 10,000 Hz. Most treatments stick to about 130 Hz, a limit borrowed from early cardiac pacemakers.
Programming takes some trial and error. Each electrode contact can act as a positive or negative pole, letting doctors shape electric fields to target problem spots and avoid healthy tissue.
Indications and Patient Outcomes
Movement Disorders have seen the most success with DBS:
| Condition | Target Brain Area | Success Rate |
|---|---|---|
| Parkinson’s disease | Subthalamic nucleus | 70-80% improvement |
| Essential tremor | Thalamus | 80-90% tremor reduction |
| Dystonia | Globus pallidus | 60-70% symptom control |
People with Parkinson’s often notice big improvements in tremor, stiffness, and slowness. Many can cut back on their meds. DBS works best for those whose symptoms improve with levodopa.
Expanding Applications are starting to show promise:
- Depression: Targets mood-regulating brain circuits
- Epilepsy: Breaks up seizure patterns
- Obsessive-compulsive disorder: Approved in Europe, with good outcomes
Picking the right patients is crucial. The best candidates have symptoms that really affect daily life but haven’t gotten relief from meds. Age, health, and expectations all play a role in success.
Most patients feel better within weeks of activation. Benefits often keep improving for months as the brain adapts.
Current Limitations
Battery life is a big headache. Non-rechargeable devices last 3-4 years before needing surgery to swap them out. Rechargeable ones last 10-15 years but need daily charging.
Replacement surgeries add to the cost, infection risk, and hassle. Newer batteries last longer but make the device bigger.
Programming is complex. Directional electrodes offer 64 contact combinations per lead. Finding the right settings takes several appointments over months.
MRI compatibility is still tricky. Newer systems allow some MRI scans, but restrictions remain on what you can scan.
Side effects can include:
- Speech issues
- Trouble walking
- Mood changes
- Infection at the surgery site
Cost is another barrier. The whole system runs £30,000-50,000, plus ongoing programming visits. Many lower-income regions just don’t have access.
Patient selection isn’t perfect yet. About 20-30% of even carefully chosen candidates don’t see much improvement. Better prediction tools would help avoid unnecessary surgeries.
Neuralink and Industry Leaders

Neuralink has become the most talked-about brain-computer interface company, with nine patients now using their wireless implants. The company stands out thanks to its advanced electrode tech and Elon Musk’s wild vision for human-AI integration.
Overview of Neuralink’s Technology
Neuralink’s N1 implant is a big leap for brain-computer interface tech. The device packs over 1,000 electrodes on ultra-thin threads that monitor brain activity in the motor cortex.
Unlike competitors like Synchron or Precision Neuroscience, Neuralink uses a fully wireless system. No external cables sticking out of the skull. Patients charge the implant every five hours with a special coil built into a hat.
Key Technical Specs:
- Electrodes: 1,000+ for high-res signal capture
- Placement: Motor cortex (more invasive than some rivals)
- Connection: Fully wireless
- Battery life: 5 hours per charge
- Surgery time: Under 2 hours with robotic assistance
The first patient, Noland Arbaugh, broke the 2017 world record for brain-computer interface cursor control speed on his first day. He now uses the device about 10 hours a day for studying, gaming, and computer control.
Elon Musk’s Vision
Musk’s vision goes way beyond just computer control—he’s talking about full-on human-AI integration. His roadmap includes robotic limbs, restoring vision, and even controlling Tesla’s Optimus robots with thoughts.
Neuralink just announced the “Blindsight” trial in the United Arab Emirates to restore vision to blind patients. Musk wants participants to control robotic arms with full sensory feedback, basically letting them “inhabit” robotic bodies.
“The future is going to be weird, but pretty cool,” Musk said at Neuralink’s summer update. He’s aiming for a “whole brain interface” that links human consciousness with AI.
This time, Musk is actually urging caution with human trials: “We’re very cautious with the Neuralinks in humans… we are taking great care with each individual.”
Major Developments in Clinical Trials
Neuralink’s clinical trials have ramped up fast across several countries. The program now runs in the US, Canada, Great Britain, and the United Arab Emirates.
Current Trial Progress:
- Total patients: 9 (as of August 2025)
- Participant profile: Paralysis or ALS patients
- Surgery locations: US hospitals only
- Recent milestone: Two patients got implants on the same day in July
The first patient had some electrode threads retract, which temporarily reduced device function. Neuralink’s team fixed the problem and published their results openly.
All participants get free surgery and implant costs, plus travel reimbursement for check-ups. The company encourages patients to share their experiences publicly—no NDAs here.
University College London Hospitals and Newcastle Hospitals got the green light for UK trials in July. This expansion helps Neuralink gather data from more diverse patients, while keeping safety standards high.
Artificial Intelligence in Neural Implants

AI is changing how neural implants process brain signals and adapt to each user. Modern algorithms decode complex neural patterns in real time and personalise responses for better results.
Adaptive Algorithms for Neural Signal Processing
Neural signals are messy and unique to each person. Old-school implants struggled to make sense of them.
AI algorithms now learn each person’s brain patterns. They filter out noise and pick up meaningful signals from thousands of impulses every second.
Key processing improvements:
- Real-time signal interpretation in milliseconds
- Reducing noise from muscle movement or outside interference
- Recognising patterns for specific intentions or movements
- Automatic calibration as brain tissue changes over time
Machine learning models keep getting smarter. They adapt as the brain changes—whether from healing, medication, or disease.
For cochlear implants, AI can pull speech from background noise in busy places like restaurants. Visual implants use algorithms to spot important objects like doorways or faces.
The tech can process up to 30,000 neural signals per second. That kind of speed allows for natural, smooth control of prosthetic limbs or communication devices.
Personalised Implant Responses
Every brain works differently, so implant settings need to be customised for each person. AI builds personalised profiles by learning the user’s unique neural patterns.
Speech brain-computer interfaces pick up on individual vocabulary and speaking habits. They start to predict common words or phrases, helping people communicate faster.
Visual implants tweak brightness and contrast based on what each user prefers. Over time, the AI figures out what’s most important—maybe it’s text, faces, or just avoiding obstacles.
Personalisation features:
- Custom sensitivity for different environments
- Learned preferences for device responses
- Adaptive interfaces that fit user abilities
- Predictive text and communication tools
Motor implants tune themselves to match the user’s intended movements. The AI learns to tell the difference between someone just thinking about moving and actually trying to move.
This kind of personalisation cuts down training time from months to just weeks. People get better control with less frustration and mental strain.
Future Potential of AI Integration
AI keeps making brain-computer interfaces smarter and more capable. In the future, implants might restore several senses at once or even boost natural abilities.
Quantum computing could someday process brain signals at incredible speeds. That might let us translate thoughts straight into speech or control several devices at once.
Emerging possibilities include:
- Memory enhancement for dementia patients
- Direct brain-to-brain communication
- Restoration of complex motor functions
- Integration with smart home systems
Wireless updates will keep implants up to date without more surgery. Developers can upgrade AI algorithms remotely, adding features or fixing bugs.
Of course, merging AI with neurotechnology brings up tough questions about mental privacy and data security. Future systems absolutely need to keep users’ thoughts safe while still delivering real benefits.
Clinical trials are already exploring implants loaded with multiple AI functions. Some of these devices could let paralysed people control computers, speak, and even experience artificial vision—all at the same time.
Cognitive Enhancement and Brain Augmentation

Neural implants aren’t just for treating medical problems anymore. They open up some pretty wild possibilities for boosting memory, improving emotional regulation, and expanding what the human brain can do.
Memory and Learning Improvement
Brain implants could help us store and recall information better. Some memory prostheses actually record neural patterns when we learn something new, then play them back later to reinforce recall.
Deep brain stimulation targets areas involved in memory consolidation. Stimulating the hippocampus during sleep, for example, can help with forming long-term memories.
Studies show that electrical stimulation can improve working memory. People with brain-computer interfaces often do better on memory tasks than they did before.
Learning speeds up, too. Transcranial stimulation synchronises brain waves in learning-related regions, so people pick up new skills faster.
But here’s the catch—these memory boosts don’t always last. The brain gets used to the stimulation, so you might need ongoing tweaks to keep the benefits.
Emotional Regulation
Neural implants can help manage emotional responses and mood disorders in ways that go beyond standard treatments. Deep brain stimulation focuses on the limbic system, which handles emotions and stress responses.
Brain-computer interfaces track emotional states in real time by reading neural activity. When they spot negative emotional spikes, they deliver targeted stimulation to help restore balance.
Anxiety and depression often respond well to specific neural stimulation. Many patients report steadier moods and less emotional volatility when their implants are set up just right.
Some systems use closed-loop feedback to automatically adjust stimulation based on what’s happening in the brain. This personalised approach can work better than one-size-fits-all treatments.
Researchers are even trying to enhance positive emotions like empathy and social connection. These ideas are still pretty experimental, but early results look promising for improving relationships and social skills.
Challenges in Cognitive Applications
Cognitive enhancement comes with some major technical and ethical challenges. Long-term biocompatibility is a big issue—implants can trigger inflammation and scar tissue over time.
Everyone’s brain is different, so it’s tough to come up with standard protocols that work for all. What helps one person might not do much for someone else because of their unique neural wiring.
Safety concerns are real, too. There’s a risk of cognitive side effects or even personality changes. Boosting memory could also make negative or traumatic memories stronger, not just the good stuff.
Neurological disorders complicate things. Conditions like epilepsy or depression can interfere with enhancement protocols, so people need tailored approaches.
Cognitive processes don’t work in isolation. If you enhance one ability, you might accidentally weaken another, leading to unexpected trade-offs.
The technology isn’t cheap and usually requires surgery, which always carries risks. That means access is limited, and there are real questions about fairness and who gets these upgrades.
Ethical Considerations and Societal Impacts

Neural implants bring up some tricky questions about privacy, freedom, and the potential for misuse. We need to sort these out before brain-computer interfaces become mainstream.
Privacy and Data Security
Neural implants gather extremely personal data straight from our brains. We’re talking about thoughts, emotions, and intentions—stuff we’ve never shared with any technology before.
What data gets collected:
- Brain signals and neural patterns
- Motor intentions and speech attempts
- Sensory processing info
- Maybe even subconscious thoughts
The biggest privacy risks revolve around who controls this data. Companies could access our most private mental info. Hackers might try to steal or mess with brain implants.
We also have to figure out data ownership. Do we own our brain signals? Can companies use them for research or profit without our clear consent?
Current protection gaps:
- Not much regulation for neural data yet
- Data storage standards are unclear
- Some devices use weak encryption
- Long-term data retention policies? Who knows
Researchers stress that accuracy and reliability matter for user safety and mental privacy. When AI processes our brain signals, strong security is a must to keep out unauthorised access.
Consent and Autonomy
Getting true consent for neural implants isn’t easy. Many people who need them have severe disabilities and may struggle to fully understand the tech.
People with locked-in syndrome or paralysis might feel like they have no other options. They may not realise how AI-driven implants could affect their thinking or even their identity.
Consent challenges include:
- Understanding long-term effects on personality
- Knowing how AI learns from brain patterns
- Figuring out what happens if the tech fails
- Grasping removal risks and procedures
We need to make sure people can make informed choices. That means explaining complex AI in plain language and giving folks time to think it over.
There’s also the issue of mental autonomy. If implants can influence thoughts or decisions, where’s the line between the device and the real you?
Some people worry that neural implants could fundamentally change who we are. Others see them as a way to restore lost abilities.
Potential for Misuse
Neural implants could be abused in ways that hurt individuals or society. The tech that helps paralysed people communicate could also be used to control or manipulate thoughts.
Possible misuse scenarios:
- Governments using implants for surveillance
- Employers demanding brain monitoring
- Enhanced people getting unfair advantages
- Criminals hacking implants for blackmail
Enhancement versus treatment is a big debate. Helping people with disabilities is less controversial than giving healthy people superhuman abilities.
This technology could increase inequality. Wealthy people might buy brain upgrades, giving them cognitive edges and widening social divides.
Military use is another worry. Brain-computer interfaces might end up in enhanced soldiers or even be used to control weapons by thought.
Regulations need to come first, not after the fact. We’ll need international agreements on enhancement limits and strict oversight of research and development.
Risks, Safety, and Limitations

Neural implants come with a lot of challenges, from surgical risks and device longevity to technical failures. These problems affect both safety and how well brain-computer interfaces work in real life.
Surgical and Medical Risks
Brain surgery is always risky, and neural implant procedures are no exception. Infection remains a serious concern, with rates hitting 5-15% in traditional deep brain stimulation.
Surgical complications can include bleeding, stroke, or damage to healthy brain tissue. Surgeons have to drill holes in the skull and go through brain tissue, which can cause immediate problems.
Device migration is another risk with wireless implants. Some can move up to 4.6mm in the first three months after surgery, which might reduce effectiveness or cause unexpected effects.
Tissue rejection is a big worry, too. The brain’s immune response can form scar tissue, blocking electrical signals or causing inflammation that harms nearby neurons.
Long-Term Viability
Neural implants need to work reliably for years, but many don’t last that long. Most batteries only go 3-7 years before needing replacement surgery.
Hardware failures happen often. Lead breakage affects about 5-15% of deep brain stimulation patients, leading to more operations to fix or swap out parts.
Encapsulation materials matter a lot for safety over the long haul. Borosilicate glass looks promising as a biocompatible choice, but we don’t have enough long-term human studies yet.
Clinical trials for neural prostheses face tough challenges tracking safety over time. Unlike other medical devices, brain implants interact with changing neural networks.
Technical Challenges
Signal quality often drops over time. Scar tissue around electrodes can make brain signals less clear, so devices may not work as well after a few months or years.
Wireless power transfer isn’t reliable yet for many uses. Current systems struggle to send enough power to deep implants without overheating tissue or causing other problems.
Data security is a growing concern as implants get smarter. Someone could hack or manipulate these devices, raising real worries about mental privacy and autonomy.
Calibration is tough, too. Brain signals vary between people and can change in the same person, so devices need frequent adjustments that don’t always work.
Future Trends and Research Directions

Neural implant technology is moving fast, with new breakthroughs tackling old problems and making these devices more accessible. Regulators are scrambling to keep up, setting clearer rules for getting new treatments to patients.
Emerging Technologies in Neural Implants
Flexible and biointegrated materials are changing the way implants connect with brain tissue. Soft electronics make better contact and reduce the mismatch between rigid devices and the brain’s delicate structure.
Researchers are working on bioresorbable electronics that dissolve safely after their job is done. This means patients can avoid risky removal surgeries.
AI integration is probably the biggest leap so far. Machine learning algorithms can now decode complex brain signals in real time, making interfaces much more accurate. These systems adapt to each patient’s unique brain patterns and get better over time.
Scientists are also building transparent electrode arrays that let them record electrical activity and do optical imaging at the same time. This dual approach gives new insight into how brain circuits work and could improve treatments.
High-density electrode arrays with thousands of recording sites are replacing old passive devices. They can monitor huge networks of neurons, which is key for restoring movement in paralysed patients.
Broadening Accessibility
Wireless neural implants are finally cutting the cord. Patients no longer have to be tethered to bulky equipment, thanks to advanced power and data transfer tech.
Manufacturing improvements are making implants cheaper. Standardised fabrication processes from the semiconductor world are bringing down costs while keeping quality high.
Developers are rolling out modular implant systems that can be customised for different conditions without starting from scratch. This saves money and speeds up getting new devices to market.
Minimally invasive insertion techniques are making surgery safer and recovery faster. Surgical robots can now place electrodes with micrometer precision, reducing tissue damage.
Training programs for surgeons and technicians are expanding worldwide, so expertise in neural implants isn’t stuck in just a few specialist centres.
Anticipated Developments in Regulatory Pathways
Regulatory agencies are now building adaptive clinical trial frameworks that give researchers more flexibility when testing neural implant technologies. With these new approaches, teams can tweak trial protocols as early results come in, which could really speed up approval times.
Teams are also rolling out risk-based approval processes just for neural implants. These frameworks accept that some people with severe conditions might need earlier access to experimental treatments, especially if nothing else has worked.
Meanwhile, international groups are working on standardised safety and efficacy requirements for different countries. This makes life easier for manufacturers but still keeps patient safety front and center.
Collecting real-world evidence is now a core part of getting these devices approved. Post-market surveillance systems follow patients over the long haul, capturing data that traditional clinical trials just can’t.
We’ll probably see more fast-track designations for neural implants aimed at serious neurological conditions with few alternatives. These faster routes could shrink development timelines from decades to just a few years for the tech that shows the most promise.
Frequently Asked Questions

Brain implants spark a lot of curiosity about safety, how they work, and what the future holds. These devices range from cochlear implants that help deaf people hear to experimental brain-computer interfaces that let paralysed patients control computers with their thoughts.
What types of brain implants are currently available?
Right now, several neural implants are already helping people. Cochlear implants have been around since the 1980s, converting sound waves into electrical signals that go straight to the auditory nerve.
Deep brain stimulation (DBS) devices help treat Parkinson’s disease and essential tremor. They act like brain pacemakers, sending electrical pulses to targeted brain areas to ease symptoms. The NHS gave the green light to DBS for Parkinson’s back in 2002.
Brain-computer interfaces are still in the experimental stage. Systems like the Utah array and BrainGate let paralysed patients control computers and robotic arms using just their thoughts. Surgeons have to implant tiny electrodes in the brain for these to work.
Myoelectric prosthetics let users control artificial limbs with nerve signals from their muscles. These don’t go in the brain, but instead connect to the peripheral nerves in the arms or legs.
How do neural implants function, and what are they used for?
Neural implants pick up, interpret, and sometimes stimulate electrical signals in the nervous system. They basically create a direct link between the brain and outside devices.
Brain-computer interfaces record neural activity when you think about moving. Then, computer algorithms decode those signals and turn them into commands for things like wheelchairs, robotic arms, or computer cursors.
Stimulation devices like DBS take a different approach. They send carefully controlled electrical pulses to specific brain regions to cut down on tremors or seizures. Doctors program these devices to target symptoms as precisely as possible.
We use these implants to restore abilities people have lost. Paralysed patients can control computers and prosthetic limbs. People with Parkinson’s often see tremors go down and movement get better.
What potential side effects might one experience with neural implants?
Any surgery comes with infection risks. The body sometimes forms scar tissue around the implant, which can mess with how well it works over time. This gliotic response can separate the device from nearby brain tissue.
Some people deal with temporary swelling or bleeding after getting an implant. Sometimes devices malfunction, and that might mean more surgery to fix or replace parts.
DBS patients occasionally notice speech issues, mood changes, or cognitive effects. Usually, these get better as doctors adjust the device settings.
Brain-computer interface users sometimes feel worn out from focusing so hard on controlling devices. The learning curve can be tough while your brain gets used to the tech.
Battery life is another thing to consider. Rechargeable systems need regular charging, and some devices require surgical battery swaps every few years.
In what ways is Neuralink advancing the field of brain implant technology?
Neuralink just finished its first human implant trial. Their chip is designed to let paralysed patients control computers with nothing but their thoughts. They mainly picked people with ALS for these early trials.
This device marks a real leap from older brain-computer interfaces. Neuralink’s system might offer more precise control and cleaner signals than what’s come before.
They’re aiming for a fully implantable system. That’s a big shift from current devices that still need wires or connectors running through the skull.
The company has big goals, hoping to treat a range of neurological conditions someday. Still, those broader uses are probably years away from actual human testing.
Can you give a brief overview of the history of brain implant development?
Neural implant research got its start in the 1950s with early cochlear implant experiments. Scientists set out to help deaf people by stimulating the auditory nerve directly.
In the late 1960s, the first myoelectric prosthetics arrived, including the well-known Boston Arm. These early versions had their limits, but they set the stage for future breakthroughs.
Cochlear implants gained FDA approval for adults in the mid-1980s. Soon after, kids started getting them too, though this stirred up debate in deaf communities about preserving deaf culture.
The 1990s brought big steps forward in brain-computer interfaces. Researchers at the University of Utah created the Utah array electrode system for visual cortex stimulation.
Deep brain stimulation came along in the late 1990s and got FDA approval for Parkinson’s in 2002. Now, thousands of patients use DBS devices.
What breakthroughs in brain implants technology can we expect in the near future?
Wireless power delivery systems are about to make a big difference—they’ll get rid of those battery replacement surgeries. That means less risk of infection and, honestly, way more comfort for patients.
Researchers keep finding better materials that work with the brain. They’re trying out new coatings to help implants blend in more naturally and cut down on scar tissue.
We’re starting to see fully implantable brain-computer interfaces show up in clinical trials. With everything tucked under the skin, these systems look better and lower the chances of infection.
Some new devices can both record and stimulate brain activity. These multi-modal tools might help treat tough conditions like depression or epilepsy, and they could work better than the old single-function implants.
Signal processing keeps getting smarter, too. Thanks to machine learning, patients may soon have much better control over prosthetic devices as the tech learns and adapts over time.

